Menu
- (206) 207-1525
- (206)207-1625
- info@seattlejawsurgery.com
Do you need to replace an entire row of teeth? In many cases our doctors at Seattle Jaw Surgery can replace an entire row of teeth in one surgical appointment. There are several ways to replace your teeth and each situation is different. Some options allow for a removable denture that is held more tightly in place by dental implants. Other options allow for a denture that is permanently fixed to the dental implants and can be removed for cleaning by a dental professional. Learning about the best option for your individual case starts with a consultation appointment with one of our doctors at Seattle Jaw Surgery. Once a method for replacement of your teeth is established, we will obtain a CT scan of your dental arches and a digital impression of your teeth. This data is used to plan for and make your new dentures. After the planning phase you are ready for surgery. Often your teeth can be removed, implants placed, and a temporary set of dentures inserted all in the same appointment.
What are my options for replacing a full arch of teeth?
It is important to realize that the following options will not work for all patients. Each treatment plan is custom tailored to the specific situation. With that in mind the general categories for full arch replacement are as follows.
Replacing teeth with implants and dentures is possible for many patients. Implants can be placed on an angle permitting use even in patients with significant bone loss. This also minimizes the need for bone grafting. If you would like to explore your options, contact our office for a consultation with one of our doctors.
The specifics of what to expect with be discussed at the consult appointment. Often sedation is used during the surgery. If this is the case, you will have to refrain from eating or drinking after midnight the night before your procedure. The duration of the surgery varies from about one hour to a few hours.
Yes. You will be on a soft diet for several weeks after surgery. It is also very important to keep the surgical area clean. You will be prescribed medications. These medications vary but often antibiotics and pain medication are prescribed. Your doctor will go over the specific instructions for medications on the day of surgery. Any questions that you may have will also be answered on the day of your surgery.
Coming Soon!
Coming Soon!
Coming Soon!
Coming Soon!
There are several pathologic processes that can be associated with the soft tissue, teeth, and bones of the mouth. Thankfully, many of these processes are benign. If you or your dentist notice changes to the soft tissue in your mouth or something abnormal on x-ray, evaluation for a biopsy should be considered. If biopsy is performed your oral surgeon may remove the entire lesion or just a portion depending on size and location. The results of your biopsy will determine what further treatment is indicated, if any. Malignant processes such as squamous cell carcinoma can also appear in the oral cavity. Biopsy of any suspicious lesion should be completed in a timely manner so that a definitive treatment plan can be rapidly developed. When a diagnosis comes back positive for malignancy, a referral to a head and neck cancer surgeon will likely be made.
Depending on the location and size of your lesion, your procedure may be completed with local anesthesia or sedation. There are many factors that contribute to this decision and the type of anesthesia is determined on a case by case basis.
Your surgery may involve complete removal of your lesion or taking a small sample of the lesion to send to a pathologist for a diagnosis. After a diagnosis is made, a final treatment plan is formulated.
The treatment for pathology varies greatly based on diagnosis and so does the recovery process. You will be given post-operative instructions on the day of your appointment and a general idea of what to expect can be determined at your consultation.
Our goal is always to preserve teeth but there are circumstances where it is just not possible to save a tooth. If you need to have a tooth or multiple teeth removed, our doctors will guide you through the process in the most comfortable way possible. We will work with your restorative dentist to formulate the best plan to replace the newly missing tooth (see here for more on implants). Ever situation is different, and your tailored treatment plan will be discussed at the consultation appointment.
The removal of your tooth or teeth may be done with local anesthesia, much like you would expect during a filling or under sedation. The type of anesthesia used will be discussed during your consultation appointment. Our primary concern is for your safety and to make the procedure and comfortable as possible. Once the teeth are removed gauze will be placed in your mouth to apply pressure at the surgical site. Depending on the situation, your gums may be closed with a stitch.
If local anesthesia was used for your extraction, then you are able to drive yourself home right away. However, if you are sedated for the surgery, you will need a responsible driver to take you home.
Yes. It is strongly recommended that you:
After wisdom teeth, the canine teeth are the next most common teeth to be impacted. The treatment for this condition varies and is often determined by your orthodontist. In some cases, the canine tooth may need to be removed. In other cases when there is space the tooth will need to be surgically exposed. An orthodontic bracket can be bonded to the tooth and a chain connected to the bracket will allow your orthodontist to aid in its eruption.
This procedure is most commonly completed under sedation in the office. After you are asleep the tooth is accessed surgically. An orthodontic bracket is bonded to the tooth and an attached chain is secured to your braces with a wire or stitch. Any incisions are closed with stitched that do not have to be removed. Later, your orthodontist with put traction on the tooth to help it erupt.
It is common to have a small amount of swelling and soreness in your mouth after this procedure. These will begin to improve after about three days in most cases. You may be prescribed medications and should take them exactly as they are written. Your oral surgeon will recommend eating only soft foods during the first several days following your procedure. It is also important to follow all instructions for post-surgical care, including cleaning the surgical site. Be sure to contact your surgeon if you experience any fever or discomfort that worsens after about three days.
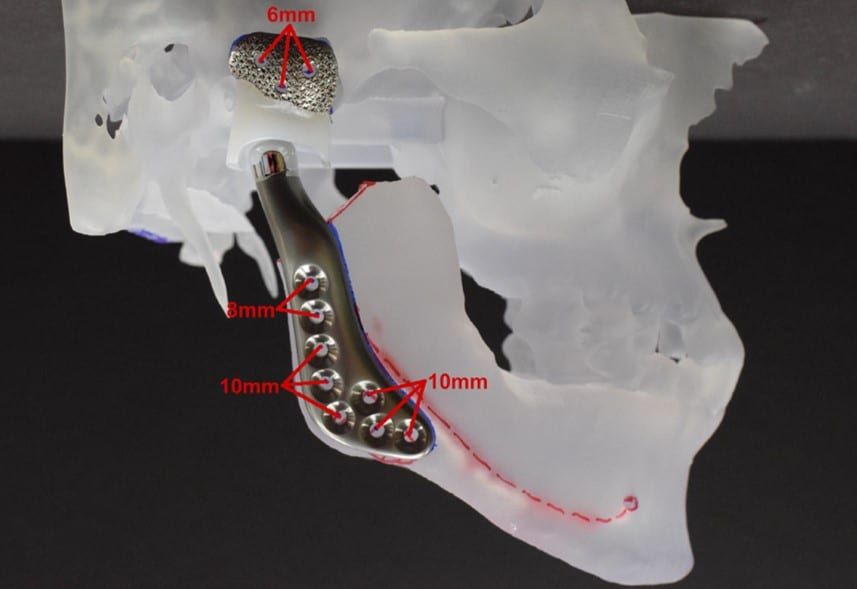
Joint replacement is a commonly performed surgical procedure. Each year in America, hundreds of thousands of knees, hips, and shoulders are replaced. For the temporomandibular joint (TMJ), it is more unusual. Many patients can benefit from the procedure. For TMJ, replacement is useful for patients with severe arthritis, severely limited mouth opening (ankylosis), joint tumors, trauma, infection, or failed previous devices.
Many times, issues with the joint can influence the overall function of the entire lower jaw. The goal for TMJ replacement is to restore function of the jaw joints. Replacing the TMJ can help reduce pain, improve mouth opening, make your upper airway bigger, correct a poor occlusion, and improve facial balance. Overall, our focus is to allow patients to improve their quality of life.
Dr. Bobek is known in the Pacific Northwest for his surgical expertise with TMJ joint replacement. He uses TMJ Concepts which fabricates custom titanium joints based on the patient’s actual anatomy. This allows for a customized and precise surgical planning with positive patient outcomes.
Recovery after joint replacement can take several weeks to months. After surgery, patients will spend 1-2 nights in the hospital and are followed in clinic with post-operative appointments at 1, 3 and 6 weeks. Patients start TMJ physical therapy about 2 weeks after surgery. At this time, they can generally return to work and begin many normal jaw functions. Given the core functions that the TMJ supports, we generally estimate that it takes 6 months before patients stabilize into their new normal state following joint replacement.
Orthognathic Surgery is the medical term for Jaw Surgery. It is a surgery to reposition the jaws to correct alignment. This realignment allows teeth to fit when misalignment cannot be solved by orthodontics alone.
Jaw surgery is completed at the hospital under general anesthesia. It is used to treat several conditions including a severe underbite or overbite, open bite, jaw or facial asymmetry, sleep apnea and others.
Typically, patients find themselves in our office after seeing an orthodontist. The orthodontist will make the recommendation based on your jaw alignment and teeth alignment if surgery may be needed in addition to orthodontic treatment to correct your bite. They would refer you to discuss orthognathic surgery with a maxillofacial surgeon.
Your initial consult in our clinic will consist of one of our surgeons taking a history, doing an examination, reviewing your clinical photos and any available imaging. They will then discuss what is involved with jaw surgery and anticipated surgical intervention. You will also be shown a cartoon demonstration video of how jaw surgery is used to reposition the jaws. After this consult you return to your orthodontist to begin orthodontic treatment.
The traditional timeline for jaw surgery patients is to be in braces for a period of time, on average this is about 6-18 months to straighten and align the teeth prior to surgery. Then the orthodontist will tell the patient when they are close to being ready for surgery. It is then that you follow up in clinic for a recall visit. One of our maxillofacial surgeons will do another exam and we will take updated photos. The surgeon will then have a better idea of what surgical treatment they recommend. At this recall if you are ready for surgery you will meet with one of our care coordinators to schedule a surgery date.
You return to clinic to obtain presurgical records. These records include an updated CT scan and an optical scan of your teeth. These are used by the surgeons to complete your virtual surgical planning (VSP). This is a way to customize the surgery to each individual patient. At your preoperative visit we will discuss the process of surgery at the hospital, review your specific plan for surgery, and review instructions for recovery after surgery.
Surgery takes place at the hospital; you spend one night in the hospital after surgery and are discharged the following day. We see you in clinic for your post operative visits at 1, 3, and 6 weeks after surgery and then 6 months after surgery.
Jaw alignment is an important part of oral health. When the jaw is out of alignment, it can negatively affect the bite, as well as the function of the mouth. Some misaligned jaws are so problematic; they cause abnormal wear on the teeth and other secondary symptoms, such as headaches. Also known as orthognathic surgery, jaw alignment surgery is meant to address irregularities that impair the normal function of the jaws. By undergoing corrective jaw surgery, patients can improve their bite, speech, and appearance – not to mention alleviate other side effects.
Though only an oral surgeon can let you know if jaw surgery is right for you, there are some signs and symptoms that the procedure could be right for you:
You may be a candidate for corrective jaw surgery if you have a malocclusion (bad bite) that is caused by poorly aligned jaws. Only a complete consultation with an oral surgeon can help you determine whether jaw surgery is right for you.
You’ll be evaluated by an oral surgeon to determine if oral surgery is right for you. In some cases, a bad bite can be treated with orthodontics alone. In others, a combination of orthodontics and jaw surgery, or jaw surgery alone is used to correct alignment issues. If you require orthodontic treatment, treatment will occur prior to jaw surgery.
X-rays will be taken of your teeth in a pre-surgical consultation. On the day of your operation, you’ll be placed under general anesthesia. An incision will be made on the inside of your mouth, through which your surgeon will reposition your jaws. Some jaw surgeries involve bone shaping, which may include shaving some bone away or grafting new bone into the jaw. A combination of plates, screws or wires may be used to hold the jaw in place before your incision is closed.
Please view our jaw surgery techniques on our videos page.
Yes. The initial healing phase is usually a few weeks long. During this time, you’ll be placed on a modified diet and instructed to avoid certain activities. It is important to take all medications as prescribed and to keep the incision site clean and free of debris. Your jaw may be swollen and sore for several days after surgery. Be sure to contact your doctor if you experience fever or any discomfort that worsens with time. Keep in mind that your jaw will continue to heal over the course of several months – a process that can take up to one year to complete.
The wisdom teeth are the final four teeth to erupt from the gums – usually sometime between age 17 and 25. Also known as third molars, these teeth can emerge and function without complication. Unfortunately, for many people there is not enough room in their jaws for the teeth to erupt and function normally. If this is the case, they can cause pain, infection, swelling or pathology. Other times they are removed to facilitate straightening of your teeth or jaw surgery. For these reasons, many people have their wisdom teeth removed.
Did you know that wisdom teeth may need to be removed even if they have not yet caused any problems? Even wisdom teeth that erupt normally may still be vulnerable to decay over time. Because of the location of wisdom teeth at the back of the mouth, many patients find it difficult to clean and floss all surfaces of the teeth each day. Although complications may not appear immediately, wisdom teeth may begin causing problems in middle to late adulthood.
You may need your wisdom teeth removed if you have one or more impacted wisdom teeth or if you are having difficulty adequately cleaning those that have emerged. It is recommended that all young adults be evaluated by an oral and maxillofacial surgeon. A consultation and x-ray can reveal impaction, damage to neighboring teeth, signs of decay, gum disease, or perceived complications with future wisdom tooth eruption.
Your wisdom teeth removal will likely be performed in your oral surgeon’s office. Most removals take only minutes to perform, but you’ll be under anesthesia or sedation to prevent discomfort. Once the teeth are removed, the gums are sutured shut. Keep in mind that you will need a responsible driver to take you home following the extraction, as it will not be safe for you to drive after being heavily sedated.
Yes. You’ll need to keep the extraction site clean and free of debris for the first couple of weeks after the wisdom teeth removal. You’ll also need to take all medications exactly as prescribed by your surgeon. Avoid sucking through a straw for the first several days after surgery, and notify your surgeon if you experience fever or discomfort that worsens after a few days.
Follow this link to watch a video summarizing these instructions.
