Menu
- (206) 207-1525
- (206)207-1625
- info@seattlejawsurgery.com
Joint replacement is a commonly performed surgical procedure. Each year in America, hundreds of thousands of knees, hips, and shoulders are replaced. For the temporomandibular joint (TMJ), it is more unusual. Many patients can benefit from the procedure. For TMJ, replacement is useful for patients with severe arthritis, severely limited mouth opening (ankylosis), joint tumors, trauma, infection, or failed previous devices.
Many times, issues with the joint can influence the overall function of the entire lower jaw. The goal for TMJ replacement is to restore function of the jaw joints. Replacing the TMJ can help reduce pain, improve mouth opening, make your upper airway bigger, correct a poor occlusion, and improve facial balance. Overall, our focus is to allow patients to improve their quality of life.
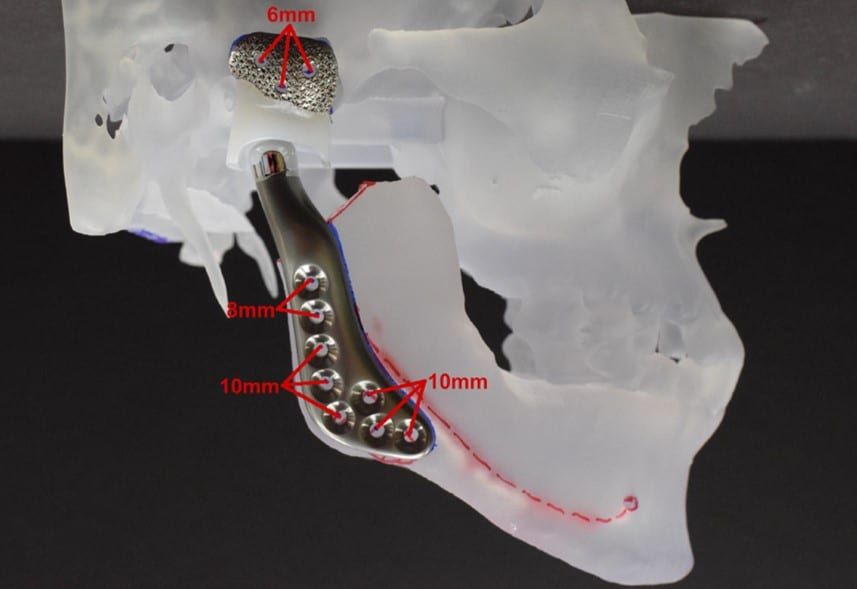
Dr. Bobek is known in the Pacific Northwest for his surgical expertise with TMJ joint replacement. He uses TMJ Concepts which fabricates custom titanium joints based on the patient’s actual anatomy. This allows for a customized and precise surgical planning with positive patient outcomes.
Recovery after joint replacement can take several weeks to months. After surgery, patients will spend 1-2 nights in the hospital and are followed in clinic with post-operative appointments at 1, 3 and 6 weeks. Patients start TMJ physical therapy about 2 weeks after surgery. At this time, they can generally return to work and begin many normal jaw functions. Given the core functions that the TMJ supports, we generally estimate that it takes 6 months before patients stabilize into their new normal state following joint replacement.
